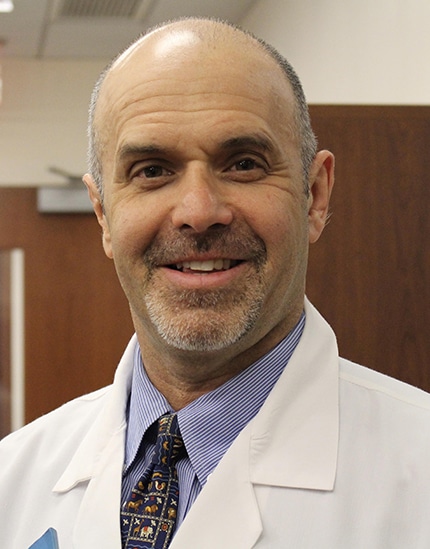
Larry Leibowitz, MD
Larry Leibowitz, MD, Board-Certified in Family Medicine, has been in practice since 1999.
Dana Murphy, MD
Board-Certified in Internal Medicine and has been in practice since 2009





Meet Our Experienced Staff Here At
Matrix Personalized Medicine
Concierge Medicine.
Personalized Care For You.
Developing a relationship with each patient is what we value most about being doctors. Our patients trust us with their health and well-being; this is a responsibility and privilege we take very seriously. Each patient and every visit is unique and should be treated with a fresh and personalized approach. In our concierge practice, we can continue providing the quality of care we have always offered our patients – with ample time to spend listening to their concerns, a strong focus on personalized attention and collaboration, and enhanced emphasis on prevention and wellness.
The office is ideally situated adjacent to New Canaan Racket Club and above Halo Studios, a health and wellness center located at 45 Grove Street.

Treating the Whole Patient
Cutting edge medicine with a personalized approach. Dr. Leibowitz combines the most current clinical advances with an unwavering focus on caring for each patient as a unique individual… mind, body, and spirit.
WHAT OUR PATIENTS ARE SAYING
Dr. Leibowitz is a very knowledgeable professional who provides excellent care.
Dr. Leibowitz is the consummate professional. He is always patient, caring and understanding. I am extremely lucky to have such a sincere, dedicated professional looking after me.
Dr. Leibowitz is wonderful!
The best doctor I have ever seen…he has a kind, caring bedside manner.
Last year I went to Dr. Leibowitz for the first time. I was immediately impressed by his calm and reassuring manner. After my recent visit I knew I had made the right choice!
I consider myself very fortunate to have Dr. Leibowitz as my primary care physician. While being extremely knowledgeable, he has the best bedside manner. More doctors should be like him!
Personalized Primary Care
Available as part of practice membership with no additional fees or copays. As a full-service concierge primary care practice, we offer routine care when you need us, as well as comprehensive annual health assessments which far exceed the traditional standards.
“DR. LEIBOWITZ IS ALWAYS VERY PROFESSIONAL, HELPFUL AND RESPECTFUL. I WOULD FOLLOW HIM ANYWHERE.”


